This section will help you to manage asthma in children aged 5-11 years.
For younger children, please see our children aged under 5 page.
For older children, please see our asthma in people over the age of 12 page.
This is not a substitute for completing an appropriate respiratory assessment module. For advice and support on choosing the right course for you, please see our training and development page.
Key facts for effective asthma management
No child should be on short acting bronchodilator (SABA) only treatment without an inhaled corticosteroid (ICS) containing inhaler. Multiple studies have shown using only a SABA to treat asthma is associated with a greater risk of fatal asthma attacks. It is essential to treat the underlying inflammation with ICS (inhaled corticosteroid) to achieve good asthma control.
Controlled asthma means children can participate in normal activities without symptoms, night-time disturbances, or using their reliever medication more than 3 times a week.
Uncontrolled asthma is defined as any exacerbation (flare up) needing requiring oral corticosteroids (prednisolone) or frequent, regular symptoms (such as using reliever inhaler 3 or more days a week or night-time waking 1 or more times a week).
Starting treatment
It is helpful to record the child’s symptoms using a validated tool such as the child asthma control test.
Start the newly diagnosed child on twice daily paediatric low dose ICS (see table 4) and a SABA for symptom relief.
You can show or send this video which explains asthma and how it is treated to the child and their family.
Choosing an inhaler device
You can use a dry powder inhaler (DPI) or a pressurised metered dose inhaler (pMDI). Remember to always provide a a spacer with a pMDI.
It is good practice to consider the environmental impact and cost of inhaler devices but you need to prescribe an inhaler which the child can, and will, use and this decision needs to be made together with the patient and their family. This might not be the most environmentally friendly inhaler but better asthma control will have a better carbon footprint than someone with poor asthma control.
Check out our guide to choosing the right inhaler and spacer.
You should document why you have chosen the inhaler, so that other HCPs will understand your decision. Remember that no changes should be made to inhaler devices without consultation with the child and their family, as this is unsafe practice. This PCRS guide explains why, and offers advice on how to balance environmental considerations with best practice.
Many primary school-aged children can use a DPI with effective training, support and practice. You can contact pharmaceutical companies for training aids to help with this.
You should consider providing an additional pMDI SABA inhaler plus spacer for emergency use for children under 12 years who might not be able to activate a dry powder inhaler during an acute asthma attack.
Demonstrate how to use the inhaler and remember to give an additional SABA and spacer for the child to take to school. If the child lives between two homes, you may want to prescribe an additional ICS, SABA and spacer.
Supported self management
Give the child an asthma action plan and upload a copy to their notes. Make sure that their parent or carer knows to share the action plan with school and any clubs that the child attends. Discuss triggers, and how to minimise contact with them, including exposure to cigarette smoke, vaping and air pollution.
For extra support, signpost the family to the A+LUK Helpline and Parent and Carer Network. Laura King and Bart’s Charity have produced a comprehensive information pack for parents and carers, with animations, all of which are available in a range of languages.
Arrange a review appointment and encourage the family to keep a symptom diary or video symptoms on their phone so that you can work out how well their treatment is working for them.
When you review them, repeat the asthma control test and ask both the child and their parent/carer about the child’s symptoms.
If asthma is not controlled
If the child’s asthma is not controlled, first of all check:
- adherence
- inhaler technique and
- any other factors that might be affecting their asthma control.
It is useful to check FeNO at this point, to see if the dose of medication is working. A low or normal reading suggests that there is no untreated inflammation present. Consider other causes for the symptoms. A high reading suggests untreated inflammation.
You can then consider stepping up treatment if appropriate, to a paediatric low dose maintenance and reliever therapy regime (MART). Explain how MART works to both the child and their family and if you are sure that they understand, then you can prescribe an ICS and Formoterol combination inhaler.
Currently only one ICS with formoterol inhaler is licensed for MART for children in this age group. It is Symbicort Turbohaler 100/6. It is licensed for children aged 6 to 11, not 5 to 11. It is a dry powder inhaler. Prescribing information can be found here. You should have completed the Tier 3 National Capabilities Framework for Professionals who Care for Children and Young People with Asthma training if you are prescribing MART for this age group.
Make sure that the child has a MART asthma action plan and that a copy of this goes to school and any clubs or childcare settings the child attends. This is important because schools and other childcare settings may not understand that the MART inhaler can be used as a reliever inhaler and may think that this means the child cannot use the school’s own SABA emergency inhaler – or that they must use it instead of their MART one.
Children aged 5-6 years
If you prescribe an inhaled corticosteroid with formoterol inhaler for a child aged 5-6 years, this will be off label.
You can explain to parents and carers that this means the inhaler is being used in a way that is not covered by its official licence. It does not mean the medicine is unsafe. It simply means you are using your clinical judgement to choose the best option for their child.
When you do this, make sure you explain it in clear language and record in the notes why you have decided to prescribe it in this way.
Learn more about prescribing off label.
For more information about devices and dosages, see this consensus guide.
You can find out more about using MART in children by listening to this PCRS webinar.
Review the child at least every 3 months. This is especially important in children so that you can be sure that the child and their caregivers are using MART effectively and safely, checking that they are not using too many additional doses. If they are regularly needing additional doses, you should refer to an asthma specialist.
If you do not think the child can manage a MART regime, then you can keep them on their ICS and SABA regime and add an 8-12 week trial of a leukotriene receptor agonist (LTRA, also known as Montelukast) instead.
Montelukast
Montelukast is taken at night time in tablet or granule form.
Ask the child’s parent/carer to keep a symptom diary during their trial of treatment.
Make sure they know to return if they have any side effects that are worrying them and ensure that you inform the family of the potential for mental health side effects. Report all suspected adverse drug reactions associated with montelukast to the Yellow Card scheme
If it is not helping or there are side effects then stop the Montelukast after (or during) the trial.
If asthma is still not controlled
Check adherence, technique, FeNO (if available) and identify any triggers, such as parental smoking/vaping and mould arising from poor housing that can be addressed. Here is a template letter that can be sent to landlords where mould or damp is an issue. If all of these factors have been considered and the child is uncontrolled:
For children on MART,
- increase their dose to paediatric moderate dose MART.
For a child who is on ICS+SABA, with or without an LTRA ,
- start them on a twice daily paediatric low dose ICS and long acting bronchodilator (LABA) combination inhaler.
Check your local formulary to find out which inhalers are licensed for children.
Update their action plan accordingly.
If asthma is still not controlled
If control is not achieved for the child on moderate dose paediatric MART, they need to be referred to a specialist, usually in secondary care. Explain to the parent/carer, and the child that they must continue with their medication whilst waiting.
Children with uncontrolled asthma who are on a twice daily paediatric low dose ICS and long acting bronchodilator (LABA) combination inhaler with or without a LTRA can be increased to a twice daily paediatric moderate dose ICS/LABA.
If this does not achieve asthma control then they must be referred to an asthma specialist, and should continue their medication while they wait.
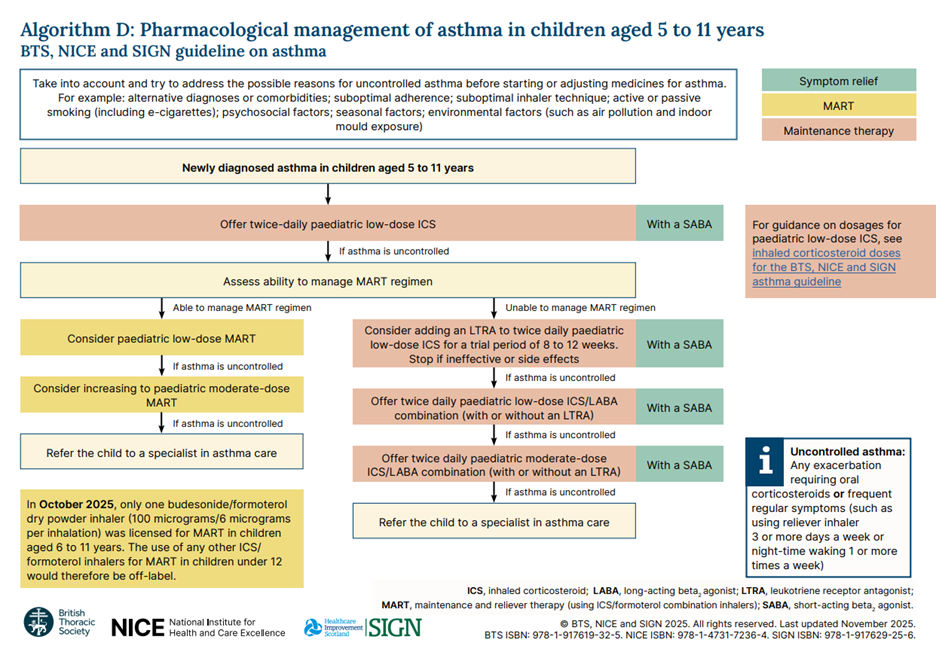
These steps are shown in the diagram below.
Stepping down
When a child's asthma has been well controlled for at least three months, it’s important to consider stepping down their therapy.
Much like inhaler choices, reducing medication must always be a shared decision, weighing the potential benefits—such as fewer side effects and a lower treatment burden—against the risk of symptoms returning.
Before stepping down, take into account how effective the treatment was when first introduced, any side effects experienced, and the child's and family’s preference.
If the child has been using a low-dose inhaled corticosteroid (ICS) alone or a low-dose maintenance and reliever therapy (MART), the next step may be to transition to a low-dose ICS/formoterol as needed.
It’s essential to agree on how this step-down process will be monitored, whether by self-assessment or clinical review, and to arrange follow-ups to ensure symptoms remain controlled. Lastly, update the child’s asthma action plan to reflect any changes in treatment and ensure caregivers know what to do if symptoms return.







