Bronchiectasis is a condition caused by damage to the lungs. On this page we’ll cover what bronchiectasis is, what causes it, what the symptoms are, and how it’s diagnosed.
On this page:
What is bronchiectasis?
Bronchiectasis is a long-term condition that affects the airways in the lungs. It’s caused by damage and scarring which make the airways wider and thicker than usual.
Bronchiectasis can happen in part of a lung or a whole lung. It can affect one or both lungs.
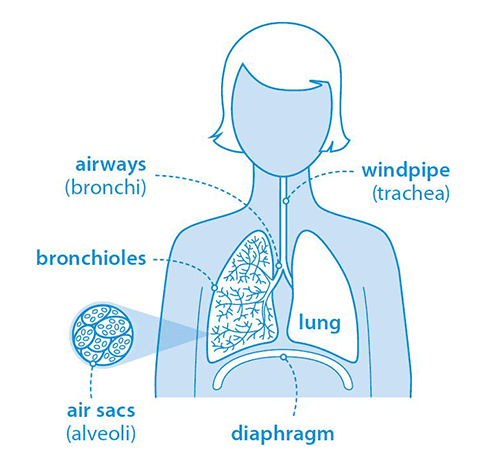
Your child’s lungs contain many airways that branch from their windpipe like a tree. These airways contain glands that produce a small amount of mucus. Mucus helps trap dust and germs. Tiny hairs called cilia move the mucus up and out of the lungs.
If your child has bronchiectasis, the airways in their lungs can’t clear themselves properly. Mucus builds up and the lungs can become infected with germs.
How common is bronchiectasis in children?
Bronchiectasis in children is uncommon. However, it is being diagnosed more in recent years. In the UK, it’s estimated that less than 1 in every 100,000 children has the condition. Bronchiectasis used to be classed as a rare disease but now doctors realise some cases were probably going undiagnosed.
What causes bronchiectasis in children?
Bronchiectasis is caused by damage to your child’s lungs. It’s important to try to work out the cause. Treating the cause can help to prevent more damage. Most often this damage is from an infection. The reason for the damage is unknown in about 4 in every 10 people with bronchiectasis.
Some causes of bronchiectasis include:
- serious infections of the lungs such as pneumonia, tuberculosis or whooping cough
- a problem with your child’s immune system (an immune deficiency) which makes them more likely to get a lot of infections
- a blockage caused by something your child inhaled, such as a small nut
- an inherited condition such as cystic fibrosis or primary ciliary dyskinesia
- your child accidentally breathing in acid that has come up from their stomach
- your child being unable to swallow safely because of a neurological issue
- a problem with the way your child’s lungs grew
- your child being born premature.
There are many other much rarer causes.
What are the symptoms of bronchiectasis in children?
The most common sign of bronchiectasis is your child coughing every day. This cough will not go away — your child will have it even when they don’t seem to have a cold or another infection. The cough might sound wet and bring up green or yellow mucus. It might improve with a course of antibiotics but will quickly return.
If your child has had a wet cough for over four weeks and this has not got better with antibiotics, they should see the doctor again.
Other symptoms can include:
- a wheezing sound when your child breathes
- tiredness
- having less of an appetite than usual
- being more breathless than usual after exercise.
Mucus is hard to digest. If your child swallows mucus, they may vomit it up. This usually makes them feel a lot better. Coughing can sometimes cause vomiting too.
Your child may have bronchiectasis if they have been diagnosed with asthma but:
- this has not got better with treatment, or
- they have lots of chest infections with green or yellow mucus.
It’s also possible to have both bronchiectasis and asthma.
Can you prevent bronchiectasis?
You can reduce the risk of your child getting lung damage that could lead to bronchiectasis. Take a look at our information on risks to children's lungs. If your child has something stuck in their lungs (a ‘foreign body’), bronchiectasis can often be prevented if this is found and removed within 14 days.
If bronchiectasis is diagnosed when in its early stages, it’s sometimes reversible. This means that with the right treatment the condition will go away. In two out of three children diagnosed, bronchiectasis can be reversed or improved.
When bronchiectasis is more severe, it can’t usually be cured but it can be controlled (stabilised) with the right treatment.
How is bronchiectasis diagnosed?
Your doctor will ask you more about your child’s medical history and their symptoms.
If your doctor thinks your child might have bronchiectasis, they’ll recommend a scan which takes an image of the inside of your child’s lungs. This scan is called high-resolution computed tomography (HRCT) and uses X-rays. Your child will need to lie still in a machine for the scan. The scan is painless and will not hurt your child.
Your doctor may recommend other tests. These are to try and find out how your child’s lungs were damaged and to help choose the best treatment.
These tests might include:
- testing your child’s mucus to see if it contains bacteria
- blood tests to check your child’s immune system
- a procedure to look into your child’s lungs using a small camera on the end of a tube called a bronchoscope
- tests on your child’s sweat to see if they have cystic fibrosis
- tests to find out if acid from your child’s stomach is going up into their lungs (this might involve inserting a tube through their nose into their oesophagus (gullet) for 24 hours to measure acid levels)
- a nose exam to look for primary ciliary dyskinesia (PCD) (this involves swabbing the inside of your child’s nose to check if the hair-like cilia for clearing mucus are working properly).
If your child has symptoms of bronchiectasis, it’s important this is investigated properly. The condition is often diagnosed later than it should be because the signs are missed.
This content is currently under review. New information will be available soon.








